The Mason-Likar 12-lead ECG
Mason Likar
The Mason-Likar (ML) system describes an alternative method for electrode placement in a 12-lead electrocardiogram(ECG). Similar to the standard ECG setup, it utilizes ten electrodes to derive twelve leads. However, the ML approach relocates three electrodes—traditionally positioned on the left and right arms and left foot—to the torso. The ML system is generally used when electrical interference from body movement is to be avoided or when positioning on the extremities is impractical.
The standard ECG: 10 electrodes - 12 leads
The standard 12-lead ECG became established worldwide during the 20th century and is also known as the 'gold standard'. It is the basis for diagnosing heart disease and the foundation of training in internal medicine and cardiology. The majority of medical studies and literature on ECG diagnosis refer to this system. Accurate lead positioning is therefore essential if the recorded ECG is to be evaluated according to the criteria of a standard 12-lead ECG. The standardized electrode positions are designed to determine the electrical activity of the heart as accurately as possible but are also partly determined by historical factors.
The development of the standard ECG recording system
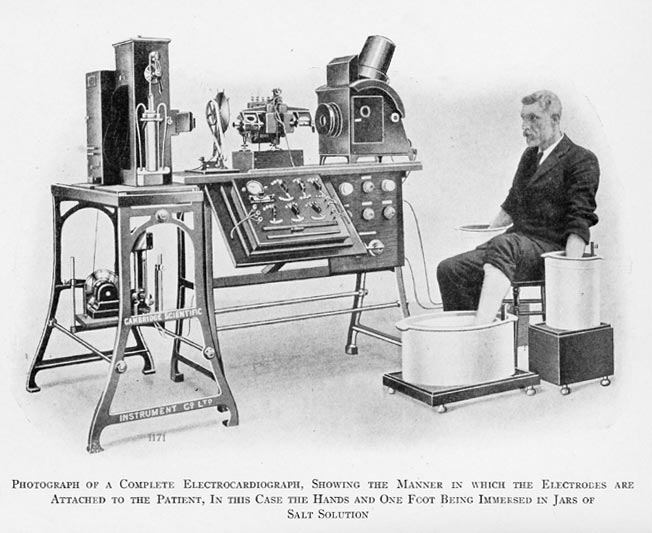
The world's first electrocardiographic recordings were made by Willem Einthoven at the beginning of the 20th century. The first three standard leads, derived from the voltage differences between the right and left arm, the right arm and left foot and the left arm and left foot, originate from his work. To measure the electrical potentials of the heart on the surface of the body, Einthoven decided to immerse the arms and the left leg in buckets of saline solution as a conductor. In the first half of the 20th century, nine further standard
leads were added to leads I, II and III: three in the frontal plane (aVR/-aVR, aVL, aVF), developed mathematically by Emanuel Goldberger in 1932 from a combination of the three previously established leads. And in 1934, six chest wall leads (V1-V6) were developed by Frank Norman Wilson, each of which is determined by an additional electrode using a virtual measuring point derived from a combination of the three foot and arm electrodes as a reference. Thus, a total of nine electrodes are used to determine twelve standard leads. The tenth electrode is used to ground the ECG device and is not used for measurement.
Susceptibility of the standard ECG to motion artefacts
The electrode placement of the standard ECG is designed for resting ECGs. When the body moves, muscle contractions generate electrical impulses that can distort the ECG graphs and make interpretation impossible. Such artefacts are particularly common in measurements from the arms and left leg. As the reference point for the unipolar chest wall leads (V1 to V6) is formed by a combination of the extremity electrodes, severe motion artefacts also occur there. However, for ECG-based diagnosis of ischemia and arrhythmias occurring during physical stress, it can be helpful to record an ECG during physical activity with limb movement.
Modified electrode placement according to Mason and Likar
Experiments with non-standard lead positions were performed as early as the middle of the last century. Although it was possible to reduce motion artefacts, the ‘angle of view’ on the heart were usually so far from the standard that many of the established diagnostic rules couldn't be applied. In 1966, Robert E. Mason and Ivan Likar presented a modified 10-electrode application system, which subsequently became the standard for exercise ECGs1.
The Mason and Likar electrode positions
Mason and Likar suggested that the electrodes, which are normally placed on the extremities, be moved to the torso to minimize motion artefacts and still ensure comparability with the standard ECG. The right arm electrode (RA) is placed in the depression below the clavicle (infraclavicular fossa), centered on the border of the deltoid muscle. The left arm electrode (LA) is placed on the left side of the upper body in the same way as RA. The left leg electrode (LL) is placed on the anterior left axillary line (a virtual vertical line from the anterior end of the armpit), midway between the lower end of the rib cage and the upper end of the pelvic bone. The positions of the chest wall electrodes remain unchanged. The ground electrode can be placed anywhere and is usually placed on the right side of the body, like LL.
Mason-Likar in practice
The modified ECG with torso-electrodes is advantageous when body movement interferes with the recording of a standard ECG. This is particularly the case when recording an exercise ECG. These are performed because some heart diseases only show up on the ECG during physical activity or are easier to detect. Coronary artery disease (also known as chronic coronary syndrome) is often undetectable on a resting ECG. Other indications include monitoring cardiac patients in hospital, performing long-term ECGs and taking ECGs in acute situations where it is often not possible to place electrodes on the extremities.
Exercise ECG
An exercise ECG is usually performed with a stationary bicycle ergometer or treadmill. The constant movement makes it difficult to obtain a clear ECG with the standard system. ML also offers the practical advantage of eliminating the need to run cables to the arms and left foot. However, in recent guidelines from the European Society of Cardiology (ESC), the exercise ECG has taken a back seat to imaging techniques as a tool for diagnosing chronic coronary syndrome2. due to its low sensitivity - the probability of a positive finding in the presence of disease is 58% - and specificity - the probability of a negative finding in the absence of disease is 62% - the ESC considers the exercise ECG to be of little value in diagnosing obstructive chronic coronary syndrome. However, the German Society of Cardiology points out in its commentary3 that it will not be possible to implement this recommendation in medical practice in Germany in the foreseeable future, as imaging techniques involve considerable additional work.

Monitoring
Another application for Mason-Likar is 12-lead ECG monitoring of hospitalized cardiac patients and long-term ECGs. In contrast to the exercise ECGs, the aim here is not to induce physical activity, but to monitor the heart continuously. However, the person being monitored is likely to be moving, which makes the use of standard electrode positions impractical. There is also a high risk of cables becoming tangled or electrodes falling off the extremities.
Standard versus ML ECG
The leads of an ECG visualize the electrical conduction within the heart, which corresponds to the contraction of the muscle tissue. For example, lead II (voltage difference between the right arm and left leg) shows the conduction process in the lower part of the left ventricle. Healthy and pathological characteristics of the ECG graphs are precisely defined for each lead. If the electrodes are positioned in a way that deviates from the standard, the axes of the examination are shifted. Applying rules based on the standard positions may then lead to incorrect diagnoses.
Discrepancies in amplitudes and axis
Numerous studies have explored the specific deviations of ML ECGs. As early as 1987, Kleiner et al. described a tendency for the axis to shift to the right in the leads of the frontal plane (I, II, III, aVR/-aVR, aVL, aVF).4 This axis shift is associated with an increase in the amplitudes in the inferior leads (II, III, aVF) and a decrease in the lateral leads I and aVL, especially the R-wave in lead I6. At the same time, there may be a loss of the Q-wave in the inferior leads and new Q-waves and an inversion of the T-wave in aVL.
Deviations also occur in the Wilson leads because these leads are based on a virtual measuring point calculated from RA, LA and LL. In leads V1, V2 and V3 the amplitudes of the Q and S waves may be reduced, while in leads V3 to V6 the amplitudes of the R wave may be increased.7
The QRS axis is used to determine the (electrical) axis of the heart in the frontal plane. It describes the direction in which the heart's electrical impulses propagate. A strong rightward shift can be interpreted as a sign of various pathologies (e.g. anterolateral infarction, septal defect). A rightward tilt due to the measurement technique could also 'correct' an actual leftward tilt of the axis and thus mask pathologies (e.g. left anterior fascicular block). The amplitudes of the ECG leads, especially the R-wave, are particularly important in the diagnosis of conduction disorders and in the diagnosis of previous infarctions. Although many of the characteristics of an ML ECG described above are significant, they may be within the thresholds for an asymptomatic ECG and may therefore be considered clinically irrelevant. However, when comparing multiple ECG readings from the same individual, using both standard and ML ECGs, these characteristics may be misinterpreted as (potentially pathological) changes in conduction.
Pseudo-inferior leads in ML ECGs?
Several studies have shown that diagnosis based on an ML ECG can lead to erroneous results in the detection or localization of infarction. A 2008 study reported the case of a hospitalized patient with a recent anterior wall infarction8. Monitoring revealed a transient ventricular arrhythmia. An ECG was recorded using torso rather than limb electrodes and showed clear new ST segment elevations in the inferior leads and corresponding ST depression in leads aVR and aVL.
This led to the presumed diagnosis of acute inferior infarction. Shortly before emergency angiography, another ECG was recorded with standard lead positions and no new infarction was observed in the inferior leads. The comparison between the ECGs was repeated: With almost identical anterior leads, the ECG with torso electrodes showed St elevations in the inferior leads, whereas the ECG with limb electrodes did not.
In 1989, a study concluded that the modified ECG failed to detect previous inferior infarctions in 69% of cases and previous posterior infarctions in 31% of cases (false negatives). In contrast, anterior wall infarcts were detected in all cases9. Given the high number of false-negative findings for inferior infarcts in ML ECGs, Papouchado et al. hypothesized as early as 1987 that the 'inferior' ML leads were modified anteroinferior leads10. This would make an ML ECG inadequate for reliable detection of inferior infarcts. On the other hand, the signs of ischemia of anterolateral infarcts could appear in the 'pseudo' inferior leads and thus lead to false-positive findings for inferior infarcts, as in the case study.
Summary
Today's standard ECG comprises twelve leads recorded by ten electrodes placed on the body. The exact positioning of these electrodes at standardized locations on the body is important for the comparability of ECG recordings and their interpretation according to learned characteristics. However, the standardized electrode positioning system is only suitable for recording an ECG at rest, as movement of the body causes electromagnetic interference in the leads, which can render the ECG unusable. The positions on the arms and the left leg are particularly susceptible to such interference, which is why Mason and Likar proposed a modified system in 1966 that places these three electrodes on the torso. Today, ML is widely employed in exercise ECGs, long-term ECGs and monitoring hospitalized cardiac patients.
However, it is essential to note that ML ECGs differ significantly from standard ECGs. Compared to the standard ECG, an ML ECG differs in some leads in the amplitudes, especially of the R-wave, and in the axis of the QRS complexes. It is important to take these characteristics into account when interpreting an ML ECG and to compare only ECGs recorded with the same electrode positions. The diagnosis of inferior infarcts may be more difficult when using modified ECGs with torso electrodes. Therefore, the modified Mason Likar system is a practical solution in situations where recording with the standard system is not possible. However, ML should not be used uncritically or to record conventional resting ECGs.
1 Mason, R.E., Likar, I. (1966) A new system of multiple-lead exercise electrocardiography. American Heart Journal, 71(2), 196–205.
2 Knuuti, J., Wijns, W., Saraste, A., et al (2020) 2019 ESC Guidelines for the diagnosis and management of chronic coronary syndromes. European Heart Journal 41,407–477. Vrints, Christiaan, Andreotti, Felicita, Koskinas, Konstantinos C., et al (2024) 2024 ESC Guidelines for the management of chronic coronary syndromes. European Heart Journal 45, 3415–3537.
3 Möllmann, H., Leistner, D. M., Schulze, P. C., et al (2020) Kommentar zu den Leitlinien (2019) der ESC zum chronischen Koronarsyndrom. Der Kardiologe 6, 482-490.
4 Farrell, Robert M., Syed, Amjad, Syed, Amina, et al (2008). Effects of limb electrode placement on the 12- and 16-lead electrocardiogram. Journal of electrocardiology, 41(6), 536–545, 537.
5 Farrell, Robert M., Syed, Amjad, Syed, Amina, et al (2008). Effects of limb electrode placement on the 12- and 16-lead electrocardiogram. Journal of electrocardiology, 41(6), 536–545, 544.
6 Toosi, Mehrdad S., Sochanski, Miroslaw T. (2008) False ST elevation in a modified 12-lead surface electrocardiogram. Journal of electrocardiology, 41(3), 197–201, 199.
7 Farrell, Robert M., Syed, Amjad, Syed, Amina, et al (2008). Effects of limb electrode placement on the 12- and 16-lead electrocardiogram. Journal of electrocardiology, 41(6), 536–545, 544.
8 Toosi, Mehrdad S., Sochanski, Miroslaw T. (2008) False ST elevation in a modified 12-lead surface electrocardiogram. Journal of electrocardiology, 41(3), 197–201.
9 Sevilla, Dorina C., Dohrmann, Mary L., Somelofski, Carolyn A., Wawrzynski et al (1989). Invalidation of the resting electrocardiogram obtained via exercise electrode sites as a standard 12-lead recording. The American journal of cardiology, 63(1), 35–39.
10 Papouchado, M., Walker, P. R., James, M. A. et al (1987). Fundamental differences between the standard 12-lead electrocardiograph and the modified (Mason-Likar) exercise lead system. European heart journal, 8(7), 725–733.