Wolff-Parkinson-White-Syndrome
Wolff-Parkinson-White Syndrome (WPW) is named after the American Cardiologists Louis Wolff and Paul Dudley White and the British Cardiologist Sir John Parkinson. They described the symptoms of WPW syndrome in young patients in 1930. In the general population, between 1 and 3 per 1,000 people is affected. WPW is often the cause of sudden cardiac death in young people.
What is Wolff-Parkinson-White Syndrome (WPW)?
What changes are present within the conduction system in WPW?
(Abgelegt unter: Marketing – Bildmaterial – Website – Blog)
What is Wolff-Parkinson-White Syndrome (WPW)?
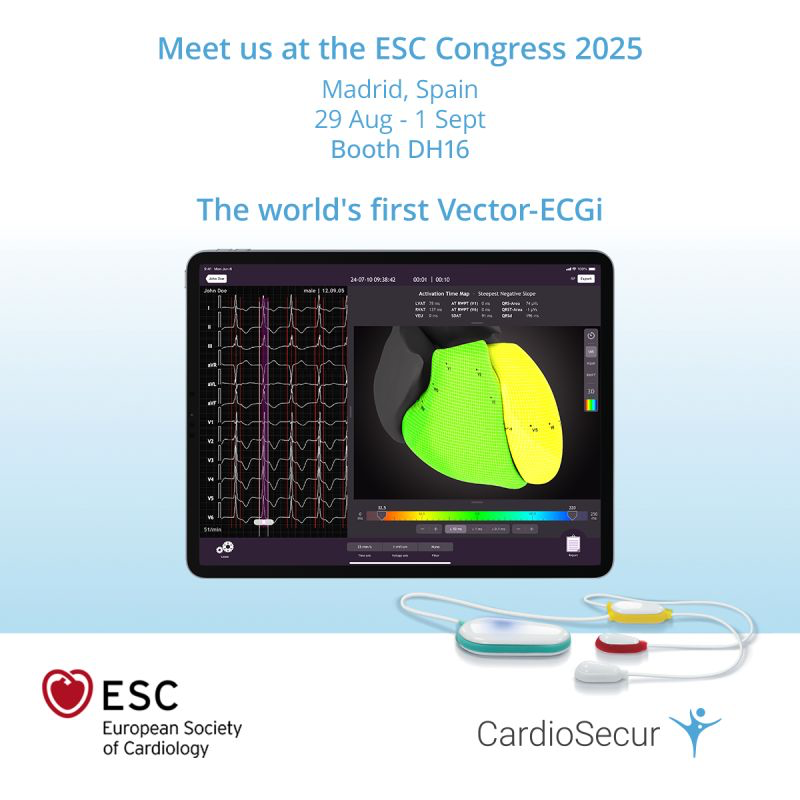
WPW Syndrome is a heart rhythm disturbance due to an anomaly of the heart’s excitation system. It is often made apparent by a sudden racing heart (tachycardia). In a healthy heart, the sinus node, located in the right atria, initiates electrical excitation. The electrical signal spreads through the atria and is then further conducted via the AV node (atrioventricular node), located between the atria and the ventricles. Between sixty and eighty impulses reach the AV node each minute. The AV node has the task of spreading the conduction to both the right and left ventricles via two conduction pathways. A normal cycle typically ends with the beating of the ventricles (image 1).
(Abgelegt unter: Marketing – Bildmaterial – Website – Blog)
What changes are present within the conduction system in WPW?
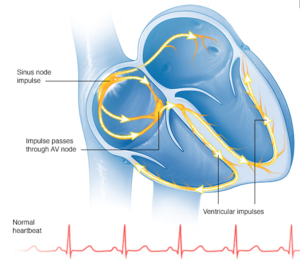
With WPW Syndrome, the excitation of the normal cardiac cycle does not end in the ventricle. Through an accessory pathway, the electrical impulse is transmitted from the ventricles back to the atria. It then triggers a new excitation of the ventricles via the AV node. This is known as a circular, or reentry, pathway (image 2). Tachycardia ensues, leading to a heart rate between 160 and 240 beats per minute. The medical term is an Atrioventricular Reentry Tachycardia (AVRT).
Accessory conduction pathways (i.e. Kent, James, or Mahaim Bundle) can conduct electrical impulses faster than the normal conduction system, thereby triggering an early excitation of the ventricles. This is known as pre-excitation and is normally harmless. However, if atrial fibrillation occurs at the same time, this can lead to a very accelerated rate, ventricular fibrillation and sudden cardiac death.
What are the symptoms of WPW?
WPW can occur without any symptoms, and is often only diagnosed by chance. However, it can also present with sudden attacks of a racing heart (paroxysmal tachycardia), which typically self-terminate just as abruptly. Those affected view these beats as harmless, but strongly annoying. Tachycardia can present both at rest and when undergoing physical exertion. When palpitations are felt, dizziness and a general feeling of unwell may follow. This can precede unconsciousness or syncope.
How is WPW diagnosed?
WPW can only be diagnosed with the help of an ECG. This shows the heart rhythm and the pathway of electrical excitation in the form of a curve. ECGs that are recorded during episodes of tachycardia are the most helpful.
WPW Syndrome has characteristic ECG changes. These include a shortening of the PR Interval (less than 0.12 seconds) and a slurred upstroke of the QRS Complex. The slurred upstroke leads to a mild widening of the QRS complex and is known as a delta wave. If a circular excitation is present, this is also called a “Circus-Movement” Tachycardia. The excitation can go in one of two ways:
- Orthodromic Conduction: track from the atria to the ventricles via the AV Node / Bundle of His System and via the accessory pathway. This is characterized by a narrow QRS complex (QRS < 0.12 s) and p waves which are visible following the QRS complex.
- Antidromic Conduction: via the accessory pathway to the ventricles and retrograde via the Bundle of His and AV Node System back to the atria. This is recognizable via a wide QRS complex (>0.12 s) and P waves that are visible after the QRS complex.
In addition to an ECG, an electrophysiological examination can be performed. In this examination, the additional pathways are localized and examined. Probes are inserted, usually via the groin, and inserted into the heart where they can measure the electrical activity of the heart.
How is WPW treated?
Treatment of WPW Syndrome is necessary when symptoms are present. The treatment options are divided into acute and chronic forms. Acute measures include drinking cold water—this stimulates the Vagus nerve (Parasympathetic nervous system), causing the racing heart to slow. Certain medications can also be administered, which must be given with simultaneous continuous ECG monitoring. It is also important to note that other medications for heart rhythm disturbances can be problematic when taken in the setting of WPW Syndrome.
A form of chronic treatment is catheter ablation, in which the accessory conduction pathways are obliterated. This is the most common form of treatment for WPW Syndrome.
Source for Images 1 and 2: www.mayoclinic.org/diseases-conditions/wolff-parkinson-white-syndrome/symptoms-causes/dxc-20266082