The Automated External Defibrillator
An automated external defibrillator (AED) is a medical device for delivering an electrical shock in specific cardiac emergencies. In contrast to manual defibrillators, an AED is intended for use by laypersons. For safe operation, an AED automatically analyzes the electrical activity and either recommends or delivers a shock when necessary. Similar to an ECG device, a defibrillator uses the fact that electrical impulses control the activity of the heart. While an ECG measures these potentials and is therefore passive, a defibrillator is active, manipulating the electrical activity of the heart to help restore a normal heartbeat.
The first Automated External Defibrillator
AED functionality and Area of Use
Use of an AED
Spread and Benefit
Medical Prerequisites for an AED Shock
Ventricular fibrillation
Pulseless Ventricular Tachycardia
History of the Defibrillator
It was first discovered in the late 18th century that electrical voltage can cause muscles to contract. During the 19th century, it was observed in animal experiments that the heart of mammals often shows a twitching or "fibrillating" movement before death, which could also be triggered by electric shocks. Experiments on dogs eventually showed that the administration of an electric shock could both induce and stop the irregular "fibrillation" of the heart and restore a normal rhythm, i.e. "defibrillate" it.
The development and widespread use of ECG technology in the early 20th century made the application of defibrillation in humans more feasible, as it provided insights into heart’s electrical activity. In 1947, the American Claude Beck performed the first successful open-chest defibrillation directly on the heart muscle using a defibrillator of his own design. The first successful closed-chest defibrillations were performed in the USA in the mid-1950s.
The first Automated External Defibrillator
In 1979, the first automated external defibrillator was launched in the USA under the name 'Heart-Aid'. Designed for use by lay people as first aiders, the device analysed the patient's heart rhythm using an integrated single-lead ECG.
The two electrodes for measuring the ECG and delivering the shock were placed on the upper abdomen and via a probe in the throat, in contrast to current practice. The throat placement was also intended to ensure patient safety: It was thought that the insertion of the probe would trigger a gag reflex in reactive individuals, preventing the treatment from continuing unnecessarily. A microphone in the tube also monitored the patient's breathing.
After automatically analysing the ECG, Heart-Aid was able to automatically deliver a shock or pace if necessary. Another new feature was that the electrodes did not have to be held in place manually. Once positioned, the probe remained in the throat. The abdominal electrode was self-adhesive. This minimised the risk of first aiders accidentally suffering an electric shock. In addition, Heart-Aid guided the first aiders through the application via loudspeaker.

AED functionality and Area of Use
The chances of survival for patients in cardiac arrest with a shockable heart rhythm are significantly improved by early shock. For this reason, guidelines and recommendations repeatedly call for the provision of automated external defibrillators (AEDs) and training in their use.1 Since the turn of the millennium, AEDs have become increasingly common in public and private places. There is little difference between the devices. They are designed so that even lay people can use them safely.
Use of an AED
According to the European Resuscitation Council, lay rescuers should use an AED after confirming circulatory arrest, making an emergency call and providing chest compressions (if possible in combination with mouth-to-mouth resuscitation), provided that chest compressions are not delayed or interrupted to obtain an AED.2 This is the case if there are several people providing assistance and an AED is nearby.

AEDs typically provide step-by-step visual and audio instructions to guide the user. An AED may be equipped with scissors to quickly expose the torso, a cloth to dry the chest and a razor for use on heavy body hair. As standard, two large adhesive electrodes are placed anterolaterally under the right collarbone and laterally under the left breast.
Once the electrodes are in place, the AED analyses the patient's heart rhythm using the built-in 1-lead ECG. This requires a pause in chest compressions, which the AED prompts with an audible (and in some cases, visual) signal. If a shockable rhythm is present, fully automated defibrillators warn the rescuer several times that a shock is about to be delivered, so that the rescuer does not touch the patient, and then automatically deliver the shock. The commonly used semi-automatic external defibrillators prompt the rescuer to deliver the shock by pressing a button. After the shock, or if there is no shockable rhythm, the device will prompt the user to continue chest compressions. Some AEDs support chest compressions by setting a rhythm. There are also systems that use sensors to analyse the depth of compressions and recommend a correction if necessary. After about two minutes, the AED will prompt the user to stop compressions to reanalyse the heart rhythm.
Spread and Benefit
Each year, between 67 and 170 out of every 100,000 people in Europe suffer a cardiac arrest outside a hospital setting.3 As defibrillation within the first three to five minutes increases the chances of survival by 50 to 70 percent, help from trained and untrained lay people before the emergency services arrive is particularly important.4
The European Resuscitation Council therefore supports the widespread provision of and education about AEDs.5 The European Society of Cardiology (ESC) also calls for AEDs to be made publicly available in places where cardiac arrests are likely to occur.6 These include shopping centres, stadiums, railway stations, airports, casinos and sports facilities. The International Liaison Committee on Resuscitation (ILCOR) also recommends that AEDs be carried on flights and cruise ships.7
The ESC also advocates the establishment of a smartphone-based alert system for first responders. This would enable trained laypersons to be quickly called to the scene of an emergency to provide first aid. According to the German Society of Cardiology (DGK), only four percent of resuscitations in Germany are carried out by trained first-aiders. However, the DGK also points out that implementing such a plan would require a great deal of effort. The DGK also points out that around two-thirds of resuscitations in Germany take place at home, not in public places.8
Medical Prerequisites for an AED Shock
Automated external defibrillators are used to treat circulatory arrest. In the event of circulatory arrest, the heart's pumping function fails so that the organs, especially the brain, are no longer supplied with blood and therefore oxygen. This is the case in cardiac arrest, but can also be the result of certain arrhythmias, i.e. an irregular, too fast or too slow heartbeat. Ventricular fibrillation, an arrhythmia characterised by particularly rapid, irregular contractions, often occurs immediately before a cardiac arrest or sudden cardiac death.
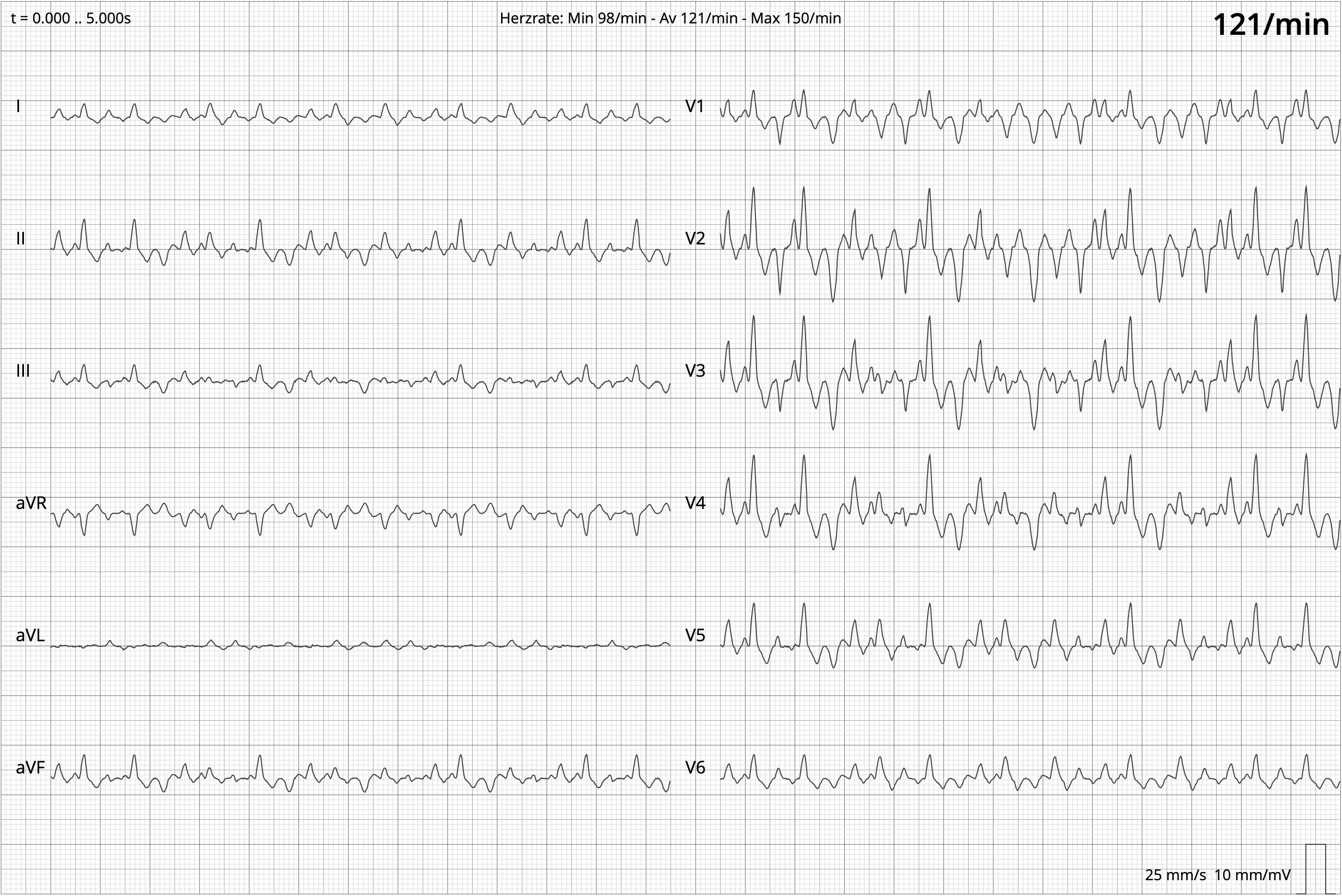
Ventricular fibrillation
An AED analyses the heart rhythm using a single-lead electrocardiogram. In two types of arrhythmia, an electrical shock from an AED can help restore a regular heartbeat. The aim of the shock is to depolarise as many heart cells as possible at the same time. This will 'reset' the heart cells and, in the best case, enable them to transmit the next electrical impulse from the heart regularly. A shock is only effective if there is still electrical activity in the heart, i.e. at least ventricular fibrillation (see Chapter 3.1). Contrary to what is often depicted in movies, defibrillators cannot restart a heart in asystole ("flat line"). They are only effective for specific arrhythmias.
Ventricular fibrillation is an arrhythmia of the heart chambers. Instead of a coordinated contraction of all the heart muscles, there is a very rapid, uneven contraction in different regions. There is no pumping and the body's circulation collapses, leading to fainting and death within a few minutes.
Ventricular fibrillation is caused by a temporary or persistent lack of uniformity in the electrophysiological properties of the cells in the ventricles. When the conductivity of areas of the ventricle is reduced, for example by scar tissue, electrical impulses are not transmitted evenly, can change direction, reactivate other areas in an uncoordinated way and thus trigger a chain reaction - known as reentry.
Ventricular fibrillation can also occur in the event of electrical accidents if the electric shock occurs at a certain point in the normal sinus rhythm: After the normal electrical impulse has been conducted by the cells through the ventricle and the heart has contracted, the cells need a certain amount of time before they are responsive to the next impulse and can trigger a heartbeat again. During this recovery phase (refractory period), some cells are still depolarised, while others can already be activated. If a sufficiently large current impulse is then applied, only some cells react, resulting in reentry and uncoordinated contractions.
In these cases, a defibrillator is used to depolarise as many cells as possible at the same time, synchronising them electrophysiologically. In the best case scenario, the next normal electrical impulse can be transmitted evenly and, together with the heart massage, lead to an effective contraction and the restoration of a pulse.
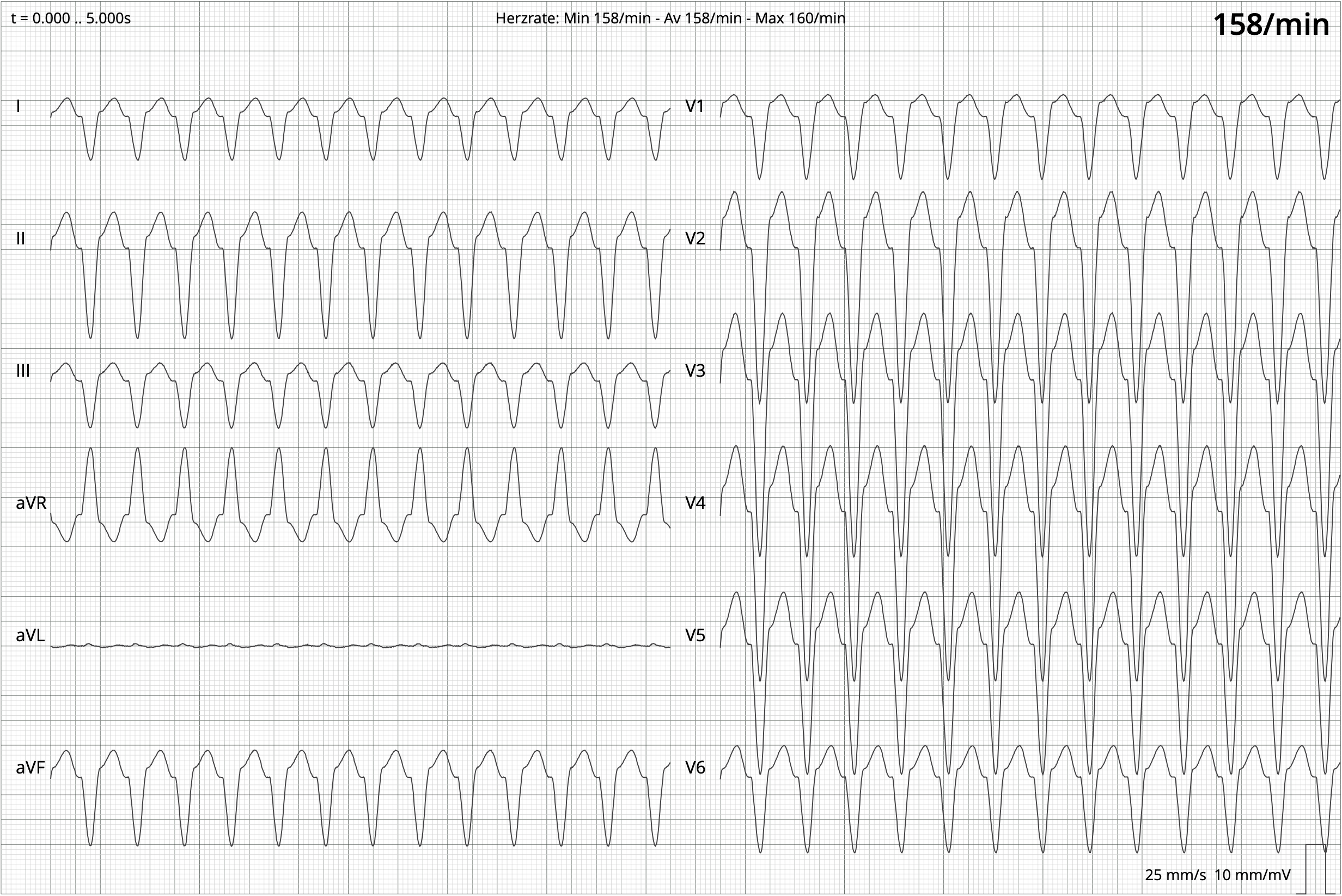
Pulseless Ventricular Tachycardia
Tachycardia is an accelerated heart rate of more than 100 beats per minute. This does not necessarily have a pathological cause; physical exertion can also cause such an increased heart rate. In ventricular tachycardia, however, the electrical impulse that reaches the cells of the ventricle does not come from the sinus node in the atrium of the heart, as is usually the case, but is generated directly in the heart chambers, the ventricles. There are also pacemaker
cells in the ventricles, but these normally have no effect on the heartbeat. However, when these cells send impulses, they can override the normal impulse from the sinus node.
In almost everyone, these cells activate a heartbeat from time to time, up to several per minute. These beats are called extra ventricular beats and are usually felt as a heart palpitation. Excitement, alcohol, other drugs and medicines can also cause extra beats. If three extra beats occur in a row, this is called ventricular tachycardia, i.e. a rapidly beating heart, the cause of which lies in the pacemaker cells of the ventricle.
Another possible physiological cause of ventricular tachycardia may be differences in the conduction and recovery phases of heart tissue, combined with the presence of scar tissue. This can lead to reentry in the ventricles, resulting in regular but much too rapid contractions. A consequence of ventricular tachycardia may be a transition to ventricular fibrillation.
Pulseless ventricular tachycardia is when the contractions of the ventricles occur so quickly that the heart does not have enough time to fill with deoxygenated blood and pump oxygen-rich blood back into the circulation. As with ventricular fibrillation, a defibrillator is used in the case of pulseless ventricular tachycardia to simultaneously depolarise the cells of the heart and make them responsive to the rhythm of the sinus node.
Other Types of Defibrillators
Besides AEDs, manually operated defibrillators are used in hospitals and emergency medical settings. The electrodes that deliver the shocks are often only placed on the body or during surgery on the heart itself. In some cases, a defibrillator can also monitor the heart rhythm, otherwise an external ECG machine is used. The energy of the shocks can be manually adjusted to suit the treatment target. By delivering an electric shock at a specific point in the heart rhythm (cardioversion), it is possible to treat arrhythmias other than ventricular fibrillation and pulseless ventricular tachycardia.
Implantable cardioverter defibrillators (ICDs) are used in patients who have a high risk of developing an arrhythmia. They analyse the heart rhythm automatically and deliver an electric shock directly to the heart tissue if necessary. As arrhythmias treated with cardioversion are not necessarily accompanied by unconsciousness, the patient may be conscious of the electric shock. ICDs can also be used as pacemakers if they are implanted directly in the heart muscle. Subcutaneous ICDs use electrodes placed under the skin rather than inside the ventricle. They are easier to implant, but require more energy for an effective shock, as the electrical energy has to pass through the tissue to the heart. Furthermore, they cannot pace, i.e. work as a pacemaker.
A defibrillator vest is used temporarily for high-risk patients. It is usually used to bridge the time until an operation, e.g. ICD implantation. These vests are also capable of cardioversion. If the device recognizes a dangerous cardiac arrhythmia, it first gives a tactile and acoustic warning. The patient can then press a button to suppress the shock, otherwise a shock is automatically triggered.
Outlook
Since the turn of the millennium, automated external defibrillators have become increasingly common in public places. They are safe to use for both patients and first responders. The effectiveness of an AED shock in preventing sudden cardiac death in ventricular fibrillation and pulseless ventricular tachycardia is undisputed. However, some concerns have been raised. For example, the DGK published a press release in 2017 questioning the balance of the cost-benefit ratio, given the small number of cases.9 In addition, the DGK warns of delays in chest compressions, which are so important for survival, when lay people first look for an AED. Given these concerns, the DGK emphasizes the need for better public education, not only on AED use but also on the critical role of effective chest compressions.
1 Semeraro, Frederico, Greif, Robert, Böttiger, Bernd W. (2021) Lebensrettende Systeme. Notfall + Rettungsmedizin 24, 367–385, Zeppenfeld, Katja, Tfelt-Hansen, Jacob, de Riva, Marta (2022) ESC Guidelines for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death. European heart journal 43(40), 3997-4126.
2 Olasveengen, Theresa M., Semeraro, Federico, Ristagno, Giuseppe (2021) Basismaßnahmen zur Wiederbelebung Erwachsener (Basic Life Support). Notfall + Rettungsmedizin 24, 386–405.
3 Gräsner, Jan-Thorsten, Herlitz, Johan, Tjelmeland, Ingvild B. M. (2021) Epidemiologie des Kreislaufstillstands in Europa Leitlinien des European Resuscitation Council 2021. Notfall + Rettungsmedizin 24, 346–366.
4 Semeraro, Frederico, Greif, Robert, Böttiger, Bernd W. (2021) Lebensrettende Systeme. Notfall + Rettungsmedizin 24, 367–385, 371.
5 Perkins, G.D., Gräsner, J.T., Semeraro, F. (2021) Kurzfassung. Leitlinien des European Resuscitation Council. Notfall + Rettungsmedizin 24, 274–345.
6 Zeppenfeld, Katja, Tfelt-Hansen, Jacob, de Riva, Marta (2022) ESC Guidelines for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death. European heart journal 43(40), 3997-4126.
7 Lott, Carsten, Truhlář, Anatolij, Alfonzo, Anette (2021) Kreislaufstillstand unter besonderen Umständen. Notfall + Rettungsmedizin 24, 447–523.
8 Eckardt, Lars, Könemann, Hilke, Bosch, R. (2023) Kommentar zu den Leitlinien 2022 der ESC zu ventrikulären Arrhythmien und Prävention des plötzlichen Herztodes. Die Kardiologie 17, 27-38.
9 Deutsche Gesellschaft für Kardiologie – Herz- und Kreislaufforschung e.V. (2017) Viele Defibrillatoren für wenige Wiederbelebungen. Pressetext DGK 10/2017.